And Surgeons
CVMS Bulletin
Making a Difference
in HealthCare for Eastern Virginia
November 2023
Volume 1, Issue 11

Thanks to all our physicians!
Thank you for all you do, day in and day out, to keep your patients healthy and to allow them to enjoy life's blessings. And even when diseases can't be cured, you always try to make the patients who have those illnesses better. You are a rare breed - people who care. People who have studied and worked hard to make things better for others. You are loved for what you do, for who you are. It can't be said enough...
Thank you!
In This Issue...
- Our First Membership Meeting
- Current Status of CVMS
- How Do mRNA Vaccines Work?
- Booster Concerns
- Loss of Physician Autonomy
- Saving the Practice of Medicine
- Barriers to Patient Care in Psychiatry
- Snapshots
- Free CMEs
- Event Board
- Newsletter Signup
Our First Membership Meeting

Mark your calendars and save the following date and place:
December 14, 2023 at 6:30-8:30 PM
The Westin Residencies Penthouse Lounge
4545 Commerce Street at Town Center in Virginia Beach
(Penthouse Entrance next to the handicapped garage directly across from the Sandler Center. Enter to Concierge Desk)
Coastal Virginia Medical Society will be hosting a Holiday Bash as its first membership meeting since its formation in January of this year. This will be a fun and entertaining evening of networking and connecting with colleagues you may not have seen for a while. There will not be a business meeting, but your hosts will be circulating to answer any questions you may have about what we are doing in the Society and what our plans are for the near future. Wine and heavy hor d'oeuvres will be served. Dr. Warth will provide a brief welcoming statement. We will also be inviting some of our newly elected representatives to engage in some of our conversations so we can learn more about each other. Bring a guest and plan to have fun - Complements of CVMS.
Current Status of
Our New Society

The Board met again on November 2. The following is a summary of what was discussed. A full copy of the minutes is available on the website.
1. We discussed in detail the time and location of our first membership meeting which will be scheduled on December 14, 6:30 to 8:30 PM with cocktails and heavy hors d’oeuvres. No business meeting will be conducted. This meeting will be primarily for the purpose of entertainment, Holiday celebration, networking, potentially meeting our newly elected representatives, and to let our members know that CVMS really exists.
2. We discussed our experience with the Medical Society of Virginia Annual Meeting in October which many of us attended. Your delegates voted appropriately for the issues we are most concerned about in our area. We learned a lot about how the advocacy program works and what we need to do to improve our approach to it next year so that we can be more effective. It is important to note that the number of our delegates is directly proportional to the number of members we have. The more members we have, the more votes we get and the more effective we are in getting our concerns addressed.
2. As part of our educational series and member benefits program, a mental health interview will be video taped soon with Dr. Jerome Blackman, Professor of Psychiatry at EVMS, regarding burnout and depression among healthcare professionals and what can be done about it.
3. We will begin production of a brief television spot on the news of each of the main three local channels to talk about medical news to develop public trust and confidence in CVMS. This hopefully with start by early next year.
4. We intend to be more aggressive in educating the public about the important health care issues that we face so that they can potentially start talking about these things with their delegates and congressmen. The average citizen doesn't really know anything about CON laws or price transparency and how it affects them. Part of our job is to inform them.
5. As we move forward into our second year, we feel we have developed a strong foundation that can and will provide a voice for all of us physicians to make a difference in our lives and those of our patients.
How Do mRNA (messenger Ribonucleic Acid) Vaccines Work?
 Courtesy of NIAID
Courtesy of NIAIDmRNA vaccines work by injecting the patient with a piece of viral mRNA found on the outer membrane of the SARS-CoV-2 virus, and other such viruses using this technology. When cells pick up these pieces of mRNA, they use them to reproduce the viral protein, which is then recognized by the immune system as a foreign substance. Lymphocytes then respond to this by producing antibodies against this foreign protein. The antibodies attach to this foreign material and destroy it. Once these antibodies are formed and the vaccinated person is later exposed to the coronavirus within the next 2-6 months, the antibodies can then destroy the virus. The difference between this and a regular vaccine is that the mRNA injection does not contain the virus. It stimulates our own cells to produce the virus protein against which our immune system then reacts.
It does not change our DNA. And it does not necessarily prevent the disease, but it theoretically helps to reduce the severity of the disease and to prevent death or hospitalization, the key word here being "theoretically." Disappointingly, it doesn't work at all for severely immunocompromised people who can't make antibodies very well. Evusheld monoclonal antibodies worked well to quash Omicron and other mutations. However, it was removed from the market when it no longer was doing its job. New protections for those autoimmune and immunocompromised patients are currently being tested in clinical trials.
What are the types of mRNA vaccines?
Healthcare providers are currently offering two types of mRNA vaccines in the United States. Comirnaty® (formerly known as the Pfizer-BioNTech vaccine) is approved for people over 12. The Moderna vaccine is approved for people over 18.
This is not new technology that was just developed for treatment of this coronavirus pandemic as many believe. For more than 30 years, scientists have been studying mRNA vaccines to prevent diseases such as:
Scientists are also studying mRNA vaccines to treat diseases like multiple sclerosis (MS)and cancer. These treatments use the same mRNA technology to trigger the immune system to create antibodies. Though they aren’t approved yet, these treatments are currently in clinical trials.
Booster Concerns
The controversy about the most recent COVID "booster" is that it hasn't been studied rigorously like we usually do with new drugs even though they may be similar to previously approved pharmaceuticals. Granted the first COVID vaccines were studied quickly and released with EUA (Emergency Use Authorization). But now, we are not in an "EUA" situation.
Many physicians are insisting that it be studied more thoroughly so we can provide our patients with true and proven information about it before we recommend it. It is not enough that it has been recommended by the CDC or the FDA. Scientific doctrine has always taught us not to assume anything. We want to see the studies that show the true statistics on the efficacy, duration of action, and the adverse effects.
Our patients need to have the full information about it before they can reasonably consent to take it, or at least be aware of the lack of information about it. I intend to take the shot because I believe that it does save lives and I don't want to be a conduit through which the disease can spread to others, but I stop short of actually advising patients to take it without them understanding this controversy. Then, it is up to them whether to take it knowing that it hasn't been studied well and we don't definitely know all the potential consequences. It's probably okay, but is that enough? If the patient develops life-threatening myocarditis from the vaccine, is that on you if you have recommended it?
Loss of Physician Autonomy
How far have
Physicians fallen in prestige and autonomy? The solo practitioner has been long
gone and only few remain. Physicians now are workers on a production line. They
have regulated hours of operation, must evaluate a set number of patients per
hour, have no control over staff hires and fires, and most importantly still
must fight for patient rights with 3rd party payers. How has this occurred?
The simple answer is that we are trained to evaluate and treat individuals
seeking help with their problems. The administrative activities of a practice
such as hiring staff, billing and collections, and meeting payrolls were never
formally introduced into our educational experience. These administrative
activities are necessary to sustain a practice, but they require extra time and
effort for a busy practitioner.
Physicians have been faced with increasing overhead costs for staff and facilities. Finding individuals with the expertise and time to manage these issues was addressed by the commitment of hospitals to take over these administrative chores. Hospitals acquired Practitioners who would be willing to have these administrative functions managed for them. Usually, the hospital system’s motive was to capture market share and control patient referrals for hospital services, building an “integrated network” where all revenue could be kept “in-house”. The Physician would now be salaried but continue to serve the patients in their practice and seek new patients. Initially there were problems in this area as Physicians saw that his/her income was set without any incentive and their work productivity declined. To increase physician productivity many hospitals began reimbursing physicians based on productivity as measured by RVU’s (relative value units) or by paying physicians a percentage of their collections.
The success of these activities was not lost to the business community who now perceived the opportunity of bundling practices for profit. Today 27% of physicians are owned by hospitals and 27% are owned by Private Equity https://www.physiciansadvocacyinstitute.org/PAI-Research/Physician-Employment-and-Practice-Acquisitions-Trends-2019-21 . In most cases electronic medical records have been transformed from a document physicians use to record pertinent findings, diagnoses, and treatments into a tool to justify billing higher fees to insurance companies and a defense against medical malpractice cases. The problems of increasing demands on Physician time by informed and knowledgeable consumers plus increasing concern regarding the time spent on meeting the goals of the electronic medical record diminish Physician-patient time and create a burden on personal time. Exactly the opposite of what was anticipated with progress in record keeping and transferring administrative issues. This trend is accelerating, and this is the time for the Physician to reevaluate their status as employer or employee and to advocate for revisions in the electronic medical record.
A recent systemic review in the BMJ highlighted the increasing Private Equity Ownership1. The Authors found marked heterogenicity in their review along with significant bias in some articles, but their conclusions indicated a consistent increase in healthcare costs, a mixed outcome in quality of health care and a shift from physician to less expensive non-physician providers. There was also a reduction in nursing staff and a shift to a lower skill set in the health care provider. Overall, there were no consistent benefits identified for Private Equity ownership. Health care today is undergoing dramatic shifts and the ownership of Physician practices, and the bundling of health care are significant issues. These changes indicate that physicians should be astute in deciding whether to stay independent or join a private equity firm. Caution is the byword.
David F. Archer, MD
November 6, 2023
1. Borsa A, Bejarano G, Ellen M, Bruch JD. Evaluating trends in private equity ownership and impacts on health outcomes, costs, and quality: systematic review. BMJ 2023;382:e075244. DOI: 10.1136/bmj-2023-075244.
Saving the Practice of Medicine
An ironic corollary to the article, "Loss of Physician Autonomy" published in this issue of the Bulletin by Dr. David Archer is that our attempt to save our practices by selling them to larger administrative organizations did not clearly provide as much benefit to many of us that we thought it would and may have made our situations worse over time. We still work as hard as we ever did if not harder. We still carry the full responsibility of patient care but we have to see more of them in less time to make a decent income. Some of the revenue we previously claimed for our practices are going to administrators. Our ability to manage our office staffs has diminished resulting in less humanitarian environments in which to practice and greater workloads for ourselves. Our office schedules are so overloaded, we can't fit patients in for urgent visits, causing loss of access to care for patients and overcrowding in emergency rooms. No one wants go into primary care any more due to inadequate pay for the usual 60-80 hour work-weeks we do, causing recruitment deficiencies and physician shortages. We have lost our respect as thinkers and problem solvers. We are only paid technicians now. And we have no influence in changing any of this.
Thus the business and bureaucracy of medicine has created a situation where physicians have lost control over their practices but yet are still fully responsible for what happens to their patients. Furthermore, they are being burdened by the extra work of maintaining lengthy EMR documents, prior authorizations, appealing decisions by insurance companies, and a myriad of other administrative details all of which are unreimbursed pressures that have very little to do with patient care and all of which raise costs and reduce time spent with patients and families. We have all the responsibilities but no control. It is easy to see how this directly links to burnout, a major problem facing physicians today.
This won't change until business, insurance, and government understand the importance of maintaining a better balance with physicians and quality patient care. We should not be assumed to be fraudulent until proven otherwise. Physicians should have more say in the workings of our health care systems. A certain percentage - at least 40% -of all healthcare administrative boards should be made up of physicians. Doctors should be salaried instead of working entirely on commissions or at least receive stipends based on service, seniority, recognition in the community, research, leadership, patient satisfaction, or a combination thereof. Dues for medical societies such as this one should be paid for by the systems that own the doctors' practices, or by the malpractice insurance providers. Leadership, humanitarianism, and business courses should be included as part of the curriculum in every medical school. This would at least be a start on the path back to normalcy.
-Greg Warth, MD, Editor
Barriers to Patient Care in Psychiatry

This is an essay about some of the problems facing psychiatrists currently. There are a host of difficulties. I will only enumerate below the matters I think are relatively uncontroversial, and comparatively serious.
The first is the problem of commitments. Civil commitment laws have been changed periodically since the 1960s. They are still far too limited, leading to unnecessary crime, homelessness, emergency rooms packed with violent, psychotic patients, and flooded family practitioners’ offices.
The second problem is the lack of psychiatric hospital beds. Many of the homeless should be hospitalized for long periods of time so they can be taken care of humanely, so they do not suffer, and so the public does not suffer either.
Again, in the 1960s and 70s, psychiatric hospitals were closed due to concerns about a “least restrictive environment” associated with patients’ civil rights. Civil rights are still important, but the pendulum has swung too far, and for this reason, all doctors, including psychiatrists, are hamstrung in being able to help very severely ill people and to protect the public. The laws need to be changed to give psychiatrists and lawyers more capacity to institute civil commitments.
The third matter has to do with insurance. Most insurance coverage for any kind of psychiatric care pays the physician less than a plumber, handyman service or an Uber driver. There’s something wrong with that picture. This problem may be impossible to rectify since “the horse has left the barn.” Nevertheless, it is almost universally agreed among psychiatrists that spending a max of 15 minutes with a patient and prescribe a psychotropic medication is far too limiting. Psychiatrists cannot get paid enough for a 45- or 50-minute psychotherapy session to survive in the United States economic environment.
The final matter that disturbs psychiatric practice in 2023 concerns malpractice liability. As it stands now, psychiatrists are responsible if any of their patients kill themselves or kill other people. It has been proven over and over for the past 50 years that psychiatrists cannot predict with any degree of certainty which patients are going to kill themselves (or kill other people), and who are not. We have a large amount of literature concerning how to try to assess suicidality in some sort of reasonable way, but all psychiatrists know that accuracy is not measurable. The laws should reflect this widely understood reality.
Professional liability for any patients who kill themselves or other people should be erased. This will allow many more psychiatrists than now to try to treat suicidal patients; as it stands, many psychiatrists have stopped accepting referrals of severely suicidal people because of the malpractice risk.
Those are some of the problems psychiatrists and their patients face. Life is full of challenges, and all of us need to live with them. But the bureaucratic difficulties impinging on the practice of Psychiatry seem to have become excessive.
Jerome S Blackman, MD
Board certified, Psychiatry
Board certified, Psychoanalysis
Virginia Beach, Virginia
Snapshots

•Vaping. A dangerous new addictive fashion accesssory and public health concern has arrived. It's a new generation of e-cigarettes or the vape du jour called Elf Bars, brightly colored e-cigarettes that look like Air-Pod cases. Bought in flavors like strawberry kiwi according to the Stanford School of Medicine an Elf Bar contains as much nicotine as 590 cigarettes. This hot new product marketed like an upscale fashion statement has begun to edge out all other like products in favor of these toy-looking pacifiers, lip-gloss, disposable e-cigarettes, and fake bcandies.
Public health experts are sounding the alarm. In your practice if you examine the mouths and throats of your patients and notice that they look unusually gray in color, your patient is vaping the equivalent of over 590 cigarettes a week. Neatly in line with maximalist aesthetic preferences of Gen Z, this is the perfect cover for nicotine products. We don't need to revisit the Nicotine Wars. We need to begin to send specific messages now that teenage vapers risk both immediate and long-term lung damage. "If it looks glamorous and it looks appealing, that's going to be the first driver that will bring the horse to water," said Brian King, the chief of the Food and Drug administration's Tobacco Center. To read more,. . . 'Cute, 'Fun' and Equal to 590 Cigarettes (NYT, 11/09/23ppD5).
• Psychiatric Drugs add pounds. What about combining one to counteract the effects of the other? What do we know about combining these medications for best responses and what do studies show?
It only seemed a natural fit, to combine the new weight loss drugs to counteract the weight gain that comes with nearly all antipsychotics and some drugs used to treat depression and anxiety.
The New York Times (11/6/23 Dani Blum) heard from 13 leading mental health facilities and psychiatric departments at major health systems in the United States. Six said they were already recommending or prescribing drugs like Ozempic to their patients. Their responses reflect a new debate in mental health care about whether to prescribe a drug patients will most likely take indefinitely, with only a limited understanding of how people with serious mental illness fare on these medications.
"We are talking about a very vulnerable population," Dr. Mahavir Agarwal, a psychiatrist and scientist at the Centre for Addiction and Mental Health in Toronto. He is conducting some of the earliest research into using semaglutide, the substance in Wegovy and Ozempic to help patients on antipsychotics lose weight. "There's next to no data," on people with depression, bipolar disorder or other mental illnesses. . .
So, as noted in the current minutes as part of our educational series and member benefits program, a mental health video series is being produced with Dr. Jerome Blackman, Professor of Psychiatry at EVMS, and CVMS Director of Public Health. Dr. Alexandria Peck Berger will ask the hard questions and fully explore physician burnout and depression among healthcare professionals.
*Physician burnout is an epidemic in the U.S. health care system, with nearly 63% of physicians reporting signs of burnout such as emotional exhaustion and depersonalization at least once per week. The American Medical Association is leading the charge on reducing physician burnout and these serious issues now face new ways to treat, approach and discuss as yet fully examined medication combinations, differing historical and newer modalities to dissect, anxiety and burnout, which may change the face and outcome of treatment minimizing physician down time and maximizing physician productivity.
As we begin writing and videotaping this series we welcome members' input and queries, with your specific questions and areas of interest that will open the dialogue needed to create a successful forum. We look forward to your comments and thoughts.
Dr. Alexandria Peck Berger
Mobile Numbers: + 1-757-333-1122,
Zoom: ialex2@aol.com.
E.: ialex2@aol.com. *
The High Cost of Healthcare:
"It's got to be the doctors who charge too much, right?" That's the typical answer from the average person on the street. The real truth is that doctors only make up 10% of the cost of healthcare. More than half the cost comes from a combination of administrative costs, and pharmaceuticals. Some of the increase may be due to the fact that patients in the US tend to be sicker because of obesity and related illnesses like diabetes, hypertension and heart failure.
Here is the recent full report on the cost of healthcare in Virginia...
Report of the Commonwealth Fund
"Pharmageddon":
This is the name of the walkout dubbed by pharmacists in Kansas City and other areas occurring in September of 2023. They are calling out unsafe working conditions that put staff and patients at risk.
Large pharmaceutical chains are closing many of their stores, laying off their staff and reducing technician hours causing burnout among the remaining staff and pharmacists. CVS is closing 900 locations. Rite Aid has closed 154 and is going through Chapter 11 bankruptcy. Walgreens closed 150 stores.
Of course this is all further reducing access to care for patients who have to wait longer for their prescriptions due to pharmacies that are much busier now and are not as readily accessible as they were previously.
Artificial Intelligence: a Two-Edged Sword
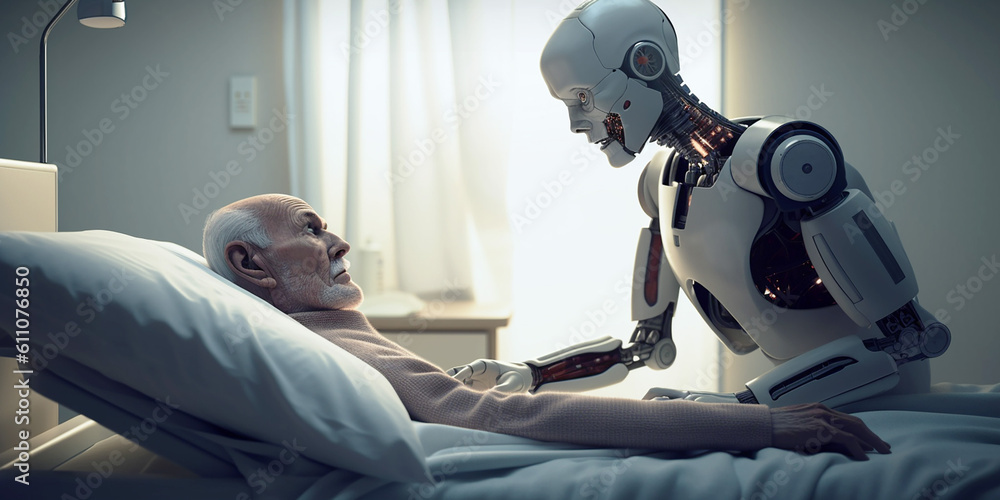
AI (Artificial Intelligence) will likely affect all of us in one way or another. On the one hand it is an excellent method of doing medical research and finding out things quickly. Before AI, we used to call this type of research "Dr. Google". Now it's much more sophisticated and will give you a few paragraphs neatly written about any disease or drug you want to know about. You can also request a differential diagnosis on a patient who with an array of symptoms, and abnormal tests which is uncannily accurate most of the time.
The problem is that it is not always accurate because it is dependent on the internet for its information. It is only as accurate as the information available in the internet, and we all know that much of the material in that resource is clouded with misinformation, disinformation, opinion, and emotion. Also much of the information obtained from AI is outdated by one or two years.
When we type in a request in Chat GPT, the request does not go to a particular database that someone has written and maintains to assure accuracy. It collects data from ALL the internet, correct and incorrect, the good and the bad, and synthesizes it into a written narrative almost instantaneously.
Even worse than that, if AI cannot find an answer to your question, it will make up something to fill the void. When humans do that, it's called confabulation. It is not accurate and cannot be relied upon as truth.
If there is more misinformation or disinformation than there is fact on the internet, AI will merely become a vehicle to spread this bad information even further compounding the problem.
We will have to be very careful not to give AI any significant control over public systems. AI cannot make judgements (yet) and probably should never be allowed to do so because those judgements will be based on potentially faulty and outdated information as long as its main resource is the internet.
If you want to use AI in your practice, you just have to realize that whatever it tells you has to be fact-checked, unless you already have the personal knowledge to know whether its statements are correct or not. And I wouldn't try to use it in court.
Other than that, it's amazing, and fast, and exciting...
just not ready for prime-time.
World Health Organization Outlines Consideration for Regulation of AI for Health
The Business of Medicine:
Hospitals and large health systems have become deeply involved in the business of medicine and perhaps less concerned about providers and patient care. This has gradually evolved over the past 30 years. Most physicians saw it coming but there didn't seem to be much we could do about it. Our incomes were being squeezed by insurance companies using DRGs under the false pretense that we were the cause of rising health costs. Many of us were experiencing high overheads and not enough revenue to keep our offices open. We fell prey to the promises of better incomes if we were bought out by hospitals. I remember thinking naively at the time that maybe they do have our interests at heart. They need us to support the hospital, to send patients there to be admitted and for testing. After all, they were making millions off the business that we were providing them. I felt a partnership developing, which I thought was good. However, a year or two after we were owned by the system, it became clear that this was not a partnership. It was a way to control us and to feed off our profits. Once that happened we became even more regulated and basically lost our ability to help manage patient care. The patients ended up being charged even more for less expensive treatments that we previously did in our offices. The cost of healthcare never improved and in fact worsened despite what we had been told. The doctors had to see more patients a day to justify their existence. The dollars were just shifted from patients and doctors to a multitude of administrators and CEOs who seem to be doing quite well as a result. Of course it was all legal. We succumbed to it. The verbiage of better patient care and community welfare was used as the rationalization for the exponential growth and monopolization of these systems, but it has become clear now that business and profits, not partnerships or patient care, is now the main focus. Patients and providers have been penalized in the process, but hey, that's on them isn't it, since they were too naive about business to see what was happening. It's survival of the fittest and the smartest in this world, right?
If this process continues unchecked, what is the future of medicine in these United States? Doctors will become mostly technicians and will be making even less income proportionately. The profession will no longer be a calling but a 9-5 job where you must be productive to be maintained. Telemedicine will take over as night or weekend call. The incentive to become a physician will diminish. The training will diminish. Patient care will diminish. Technicians will be using AI to treat hundreds of patients per day. Malpractice suits will increase. As patient care and lengths of stay get squeezed more and more, doctors will have even less say about what happens to their patients. The only path to success for those starting out in medicine will be to obtain an additional degree as an MBA or JD.
The only way we can get out of this mess is to ask our lawmakers to help. There are so many things that have developed over the years that have cumulatively caused an undue burden on patients and providers. We need to try at least to change some of these things to balance the situation. We cannot do it alone. We need hundreds of physicians to band together, to inform the public about what is happening and to request our representatives and delegates to support us. The only way to do that - the only mechanism we have - is through our medical societies.
If you have not already joined as an active member of our society, please do so now so you can have a voice in the future of healthcare in Virginia.
Read more...
Easy, Free, Educational CMEs
The non-profit CME Outfitters provided by Alosa Health has developed an easy, online, free program for clinicians to not only satisfy your CME obligations, including the required opioid certification, but also to get other educational, practical CMEs that make a real difference in patient outcomes.
Click here...https://www.cmeoutfitters.com/transfers/cm/?ID=45805
CVMS Event Board
Your Comments
Please add your comments or suggestions on any past or future events in the box below.
Newsletter
Stay up to date on issues and news you need to know. The CVMS Bulletin is published monthly and will list concerns that local physicians have expressed about healthcare in Coastal Virginia and how we can make it better. We will provide potential solutions and let you know what is happening behind the scenes to help solve these problems. Membership is not currently required to receive the newsletter.
We hope you enjoyed this new edition of the CVMS Bulletin. If you have any questions, concerns or comments, let us know at admin@cvmedicalsociety.org. If you wish to provide an article or your own story to put in this newsletter, send it in. Watch the "What's New" link in the upper left Navigation Menu for updates in between the monthly newsletters. Let us know if you wish to be involved in the CVMS organization process or if you know of any resources or benefits we could potentially provide for the membership.
Thank you for subscribing to the CVMS Bulletin.


Recent Articles
-
CVMS-Bulletin-November-2025
Nov 28, 25 08:23 AM
CVMS Newsletter - Medical News and Commentary -
CVMS Membership Drive 2025
Oct 16, 25 10:53 AM
Information about the membership importance and benefits. -
Letter to Governor Youngkin re: COVID-19 Vaccine Recommendations
Oct 16, 25 10:45 AM
The Honorable Glenn Youngkin
Office of the Governor
P.O. Box 1475
Richmond, VA 23218
Dear Governor Youngkin,
On behalf of the Coastal Virginia Medical Society (CVMS), based in the Hampton Roads area of Sou…
Sign Up for the New CVMS Bulletin
Things You Need to Know
News Releases
from the
Virginia Beach Health Department
Norfolk Public Health Department
Chesapeake Health Department
The Roman Fasces was a symbol of strength and power occurring as a result of many binding together. It was made of multiple elm or birchwood rods about 5 feet long tied together and sometimes including an axe. It was carried by attendants to soldiers or powerful figures in ancient Rome. For us, it symbolizes that we are stronger and more powerful if we bind together in supporting our goals.







